Today, Susan G. Komen, the world’s largest nonprofit funder of breast cancer research, announced new grants to 124 researchers in 25 states and eight countries internationally, with about half of the grants targeted to early-career researchers squeezed by stagnation in federal research dollars.
The grants include more than $447,000 in new funding for research at Washington University School of Medicine, bringing Komen’s total research investment in Missouri to $22,372,092 since 1982.
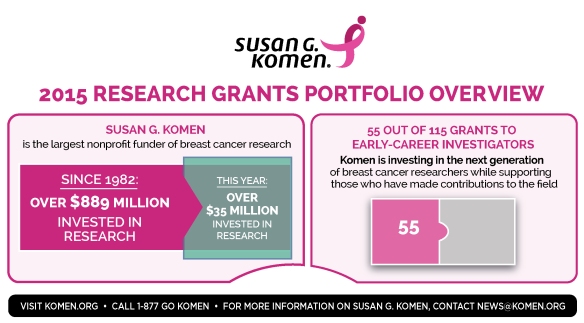
The 2015 research grants expand Komen’s ongoing commitment to funding early-career scientists, that is, recent graduates and those trying to establish independent research careers. This group has been especially hard hit by real-dollar declines of as much as 25 percent in federal research funding over the past decade.
“We committed two years ago to do all that we can to ensure that talented early-career investigators remain in the breast cancer research field, while continuing our support for established researchers,” said Komen President and CEO Judith A. Salerno, M.D., M.S. “We cannot afford to lose talented scientists to other fields for lack of funding.”
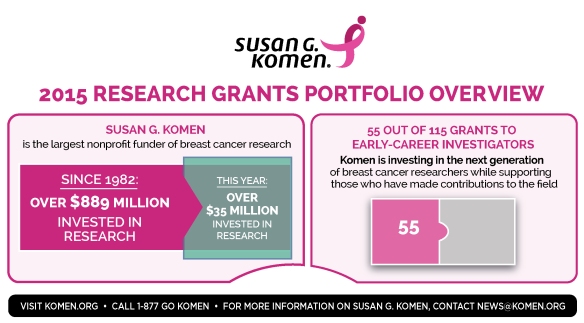
This year’s research slate brings Komen’s total research investment to more than $889 million since 1982, the largest of any nonprofit, and second only to the U.S. government.
Grants from Komen’s nearly $36 million research portfolio – including more than $17.6 million in grants awarded to early-career investigators – span the entire cancer continuum from prevention to treatments for aggressive and metastatic disease. These include:
- 36 grants to improve understanding of metastatic breast cancer
- 18 grants investigating how tumors develop drug resistance
- 19 grants related to the study of triple negative breast cancer – one of the most aggressive forms of the disease
- 15 grants working to identify and understand biological and socio-economic health inequities
- 13 grants seeking to develop new and novel therapies
Komen’s Investments in Missouri
Komen’s research program is funded in part by contributions from Komen’s nationwide network of Affiliates, which direct 25 percent of locally raised funds to Komen’s national research program. The remaining 75 percent of net funds are invested into community outreach programs that serve local women and men facing breast cancer.
“We are so proud to have the support of this community as we help our friends, coworkers and neighbors who are facing breast cancer, and work for continued progress against breast cancer through research,” said Helen Chesnut, Komen St. Louis executive director.
In Missouri, more than $452,000 will be invested into breast cancer research efforts in the state.
These funds include more than $447,000 to Adetunji Toriola, M.D., Ph.D., of Washington University School of Medicine to investigate the relationship between mammographic density and the RANK pathway, which was recently demonstrated to play an important role in the growth of breast cell types that contribute to breast density in pre-clinical studies and therefore may impact breast cancer risk.
A full list of Komen’s 2015 research grants can be found here. (Grants are contingent upon signed and executed contracts with Komen.)
In addition to funding breast cancer research, Komen has invested more than $1.95 billion into community health outreach and global programs that serve hundreds of thousands of women and men annually through breast cancer health and support programs that screen, educate and provide financial, medical and psychosocial assistance.
For more information about Komen’s mission investment, please visit komen.org.
For more information about Komen St. Louis, please visit komenstlouis.org.
 In the past, many women used menopausal hormone therapy (MHT) to relieve hot flashes and other symptoms of menopause. But studies show that use of estrogen plus progestin increases the risk of both developing and dying from breast cancer.
In the past, many women used menopausal hormone therapy (MHT) to relieve hot flashes and other symptoms of menopause. But studies show that use of estrogen plus progestin increases the risk of both developing and dying from breast cancer.